Asthma is a common lung condition that causes occasional breathing difficulties.
It affects people of all ages and often starts in childhood, although it can also develop for the first time in adults.
There’s currently no cure, but there are simple treatments that can help keep the symptoms under control so it does not have a big impact on your life.
Please note that asthma in CHILDREN is different to asthma in children aged 12 and above and ADULTS. The treatment and management plans are different. Click here for advice for children and young people with asthma. Asthma is a serious condition and can lead to death if not managed appropriately.
See transcript of above advice
Hello everyone, I am Amir Hannan, a GP at Haughton Thornley Medical Centres
And I am Punam, our Senior Clinical Pharmacist.
We’re here to discuss some significant updates regarding asthma management that are essential for you to understand. These changes are being implemented by experts in the field, and they are designed to improve the way asthma is diagnosed and managed, as well as to guide you on what to do in the event of an asthma attack. Our goal is straightforward: to enhance your care, prioritise your safety, and ultimately save lives.
Asthma is more prevalent than you might think. In the UK alone, 7.2 million people are living with this respiratory condition, which equates to about 8% of the population. At our practice, we manage asthma for more than 2000 patients out of a total of nearly 13000. In addition Tameside has the highest level of asthma admissions across Greater Manchester and patients stay in hospital longer than elsewhere. Those living with asthma often experience symptoms such as wheezing, shortness of breath, persistent coughing, or a feeling of tightness in the chest. These symptoms can vary in severity and sometimes escalate rapidly, leading to an asthma attack. You might find that different factors trigger your symptoms—these can include exercise, allergens, and even changes in the weather. Each individual with asthma has unique triggers, which means it’s vital to understand and manage your condition accordingly.
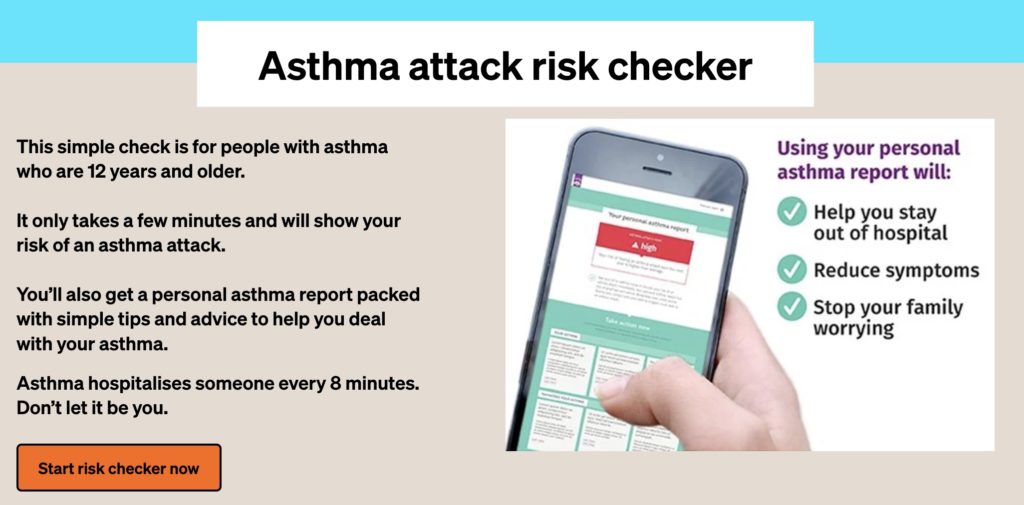
Currently, while there is no cure for asthma, most individuals can successfully control their symptoms using asthma inhalers and various medications. It’s worth noting that some people may go several weeks or even months without experiencing any symptoms. However, the statistics surrounding asthma are concerning, with four individuals dying each day in the UK due to asthma attacks, the majority of which are preventable. The most effective way to reduce your risk is by adhering to your prescribed asthma medications, even when you’re feeling well, and having an asthma action plan in place can significantly improve your management.
Now, let’s talk about the changes we’ve made. We now have the ability to diagnose asthma more effectively using a straightforward blood test that can help confirm your diagnosis. If you’ve already had this test recently, you might not need to repeat it. Alternatively, our nurses can conduct a quick FENO test that only takes about five minutes. If required, we will ask you to monitor your peak flow readings twice daily to track variations, or we might request a more formal spirometry test. In rare cases where we are unsure about the diagnosis, a referral to a hospital for further specialist testing may be necessary.
One of the most significant adjustments in asthma management is related to treatment protocols. We are moving away from the traditional use of salbutamol inhalers for managing asthma attacks. For patients with well-managed asthma, we now recommend alternatives such as DuroResp, Symbicort, or WockAir. You can take one puff of these inhalers up to six times in a single instance if you’re experiencing symptoms, and you may use them as a reliever medication up to eight times a day as needed.
If you find yourself needing to use your inhaler more frequently, we recommend that you take one puff of DuroResp, Symbicort, or WockAir twice daily while also keeping the option available to use up to six doses for immediate relief. In situations where you continue to experience symptoms, your doctor may advise increasing your intake to two puffs twice daily while still allowing for the usual reliever doses. Depending on your circumstances, you may also be prescribed additional medications such as Montelukast or Spiriva Respimat.
As the phased transition away from salbutamol takes place, we are focused on ensuring that patients are adequately supported during this change. It’s not just up to the doctors; our pharmacists and nurses are here to help you, particularly if your asthma is not well controlled. We will help guide you through adding new medications and adjusting your treatment plan to better suit your needs.
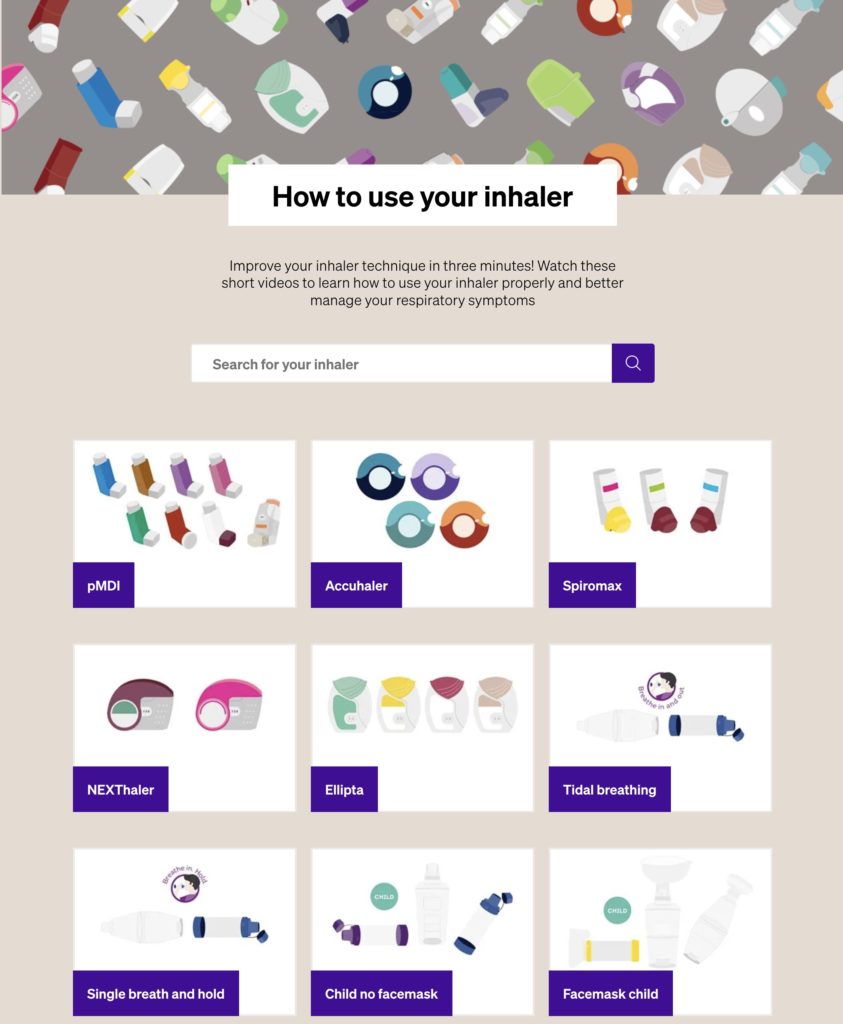
Furthermore, we encourage the use of dry powder devices for inhalation therapy. These devices are more environmentally friendly and help to decrease our carbon footprint. While some patients may initially find these devices less familiar, with practice, you will adapt, and many will find them easier to use. Remember all inhalers taste and feel different and it may take time to get used to them.
If you’d like to learn more about managing your asthma effectively, there are plenty of resources available on our dedicated asthma care page. We are committed to ensuring you have access to the information and support you need as you navigate these changes.
Remember, these modifications to how we approach asthma care are aimed at you—at enhancing your quality of life and safeguarding your health. We are here to assist you every step of the way. Thank you for taking the time to listen, and we look forward to helping you manage your asthma more effectively.
“Our goal is straightforward: to enhance your care, prioritise your safety, and ultimately save lives. We are no longer prescribing the blue inhaler (salbutamol / ventolin) as reliever therapy for asthma in adults as there is a better alternative for you”
Dr Amir Hannan, GP
We NO LONGER recommend the BLUE inhaler (salbutamol) for adults aged 12 and over. Please speak to your doctor, nurse or pharmacist who advise you about the new AIR or MART treatments as described below following the new NICE guidance
AIR (anti-inflammatory reliever)
If you only get asthma symptoms occasionally, your doctor or nurse may prescribe you an anti-inflammatory reliever inhaler, known as AIR to use only when you need to.
Maintenance and Reliever Therapy (MART)
Find out more about anti-inflammatory reliever (AIR) and Maintenance and Reliever Therapy (MART), when your doctor or nurse might prescribe MART, and how it can help your asthma symptoms.

What is asthma
What to do if you are an adult aged 12 or over and have an asthma attack and are on the NEW AIR or MART Asthma Management plan
Click here to learn what to do if you have an asthma attack (for adults aged 12 and above)
What to do if your child has asthma attack
Asthma attack advice for a MART inhaler
- Sit up – try to keep calm.
- Take one puff of your MART inhaler every 1 to 3 minutes up to six puffs.
- If you feel worse at any point OR you do not feel better after six puffs, call 999 for an ambulance.
- If the ambulance has not arrived after 10 minutes and your symptoms are not improving, repeat step 2.
- If your symptoms are no better after repeating step 2, and the ambulance has still not arrived, contact 999 again immediately.
If you do not have your MART inhaler, call 999 straight away.
Asthma attack advice for an AIR inhaler
- Sit up – try to keep calm.
- Take one puff of your AIR inhaler every 1 to 3 minutes up to six puffs.
- If you feel worse at any point OR you do not feel better after six puffs, call 999 for an ambulance.
- If the ambulance has not arrived after 10 minutes and your symptoms are not improving, repeat step 2.
- If your symptoms are no better after repeating step 2, and the ambulance has still not arrived, contact 999 again immediately.
If you do not have your AIR inhaler, call 999 straight away.
I do not have a reliever inhaler
If you do not have your reliever inhaler, and you’re struggling to breathe, call 999 straight away.
Do not wait to see if you get better on your own. An asthma attack makes it hard to breathe, which is a medical emergency. You must get the reliever treatment you need quickly.
- Sit up and try to stay calm.
- Call 999 for an ambulance.
- Tell the call handler that you do not have a reliever inhaler with you.
NHS Choices in adults
The Greater Manchester Medicine Management Asthma plan provides a step by step advice for children aged over 12 and adults
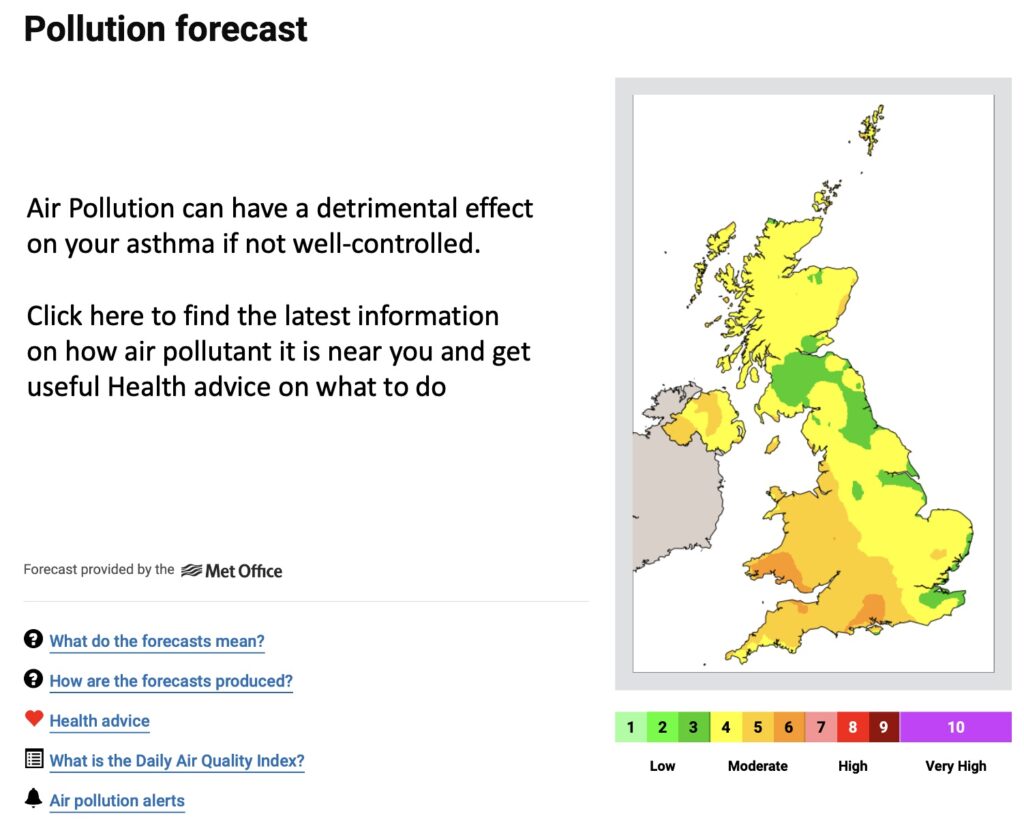
Find out how air pollution affects your lung condition, the risk from different types of pollutants, when and where air quality is likely to be worse, and what you can do to limit the effects
Learn more for adults
NHS Choices: Asthma in Adults
Patient.co.uk: Asthma in Adults
Learn more for children
Patient.co.uk: Asthma in children
Asthma in Children – talk by Dr Levy, consultant paediatrician with an interest in asthma